Future-Proof Hospital Design: Why Indian Healthcare Facilities Need Adaptability, Not Predictions
Today’s Solutions Become Tomorrow’s Constraints
Every hospital designed in 2025 solves today’s problems perfectly. The crisis emerges 5-10 years later when those solutions become rigid constraints. A 200-bed facility built in 2015 designed its ICU for 60 beds—adequate for cardiac cases and post-surgical care. By 2020, COVID demanded more ICU beds. Their options: spend ₹1.2 Cr on disruptive renovation with 4 months downtime, operate overcapacity with beds in corridors risking accreditation penalties, or turn away critical patients eroding referral physician trust.
If that hospital had been designed with flexibility in mind, the “renovation” would have been a 2-week reconfiguration costing ₹8-12 lakhs. That’s the cost of rigid design—and it’s bankrupting Indian hospitals that prioritized construction efficiency over operational adaptability.
Five Unstoppable Forces Reshaping Indian Healthcare
These aren’t predictions—they’re present realities accelerating over the next 15 years:
1. Demographic Tsunami
India’s 60+ population is projected to double by 2050, from 140 million to 280+ million. This drives exponential demand for chronic disease management, oncology, dialysis, cardiac care, and geriatric rehabilitation. Your current bed mix and department sizing will be wrong within 5 years.
2. Technology Disruption
AI diagnostics already outperform radiologists in specific domains—imaging workflows will transform. Surgical robotics are moving from niche to mainstream, changing OT ceiling height and equipment weight requirements. Hybrid PET-MRI and interventional suites require structural load capacity most hospitals don’t have. Telemedicine demands IT infrastructure density 10x what was adequate in 2020.
3. Disease Burden Evolution
Lifestyle diseases (diabetes, hypertension, obesity) are India’s new epidemic—outpatient volumes will surge. Infection spikes (COVID won’t be the last) make rapid conversion to isolation or ICU capacity a survival imperative. Precision medicine changes pharmaceutical storage, lab configurations, and treatment protocols.
4. Care Model Transformation
Procedures migrate to day care, shortening inpatient stays—today’s 30-bed ward could need to be 15 beds plus 10 recliners tomorrow. Home-based care integration means hospitals become hubs, not destinations, shifting space needs. Value-based care penalizes inefficiency, making operational flexibility financial survival.
5. Regulatory Acceleration
Safety standards tighten (fire, infection control, accessibility). Energy efficiency mandates increase (green building codes, carbon neutrality targets). Accreditation requirements evolve every revision cycle.
The hard truth: A hospital designed as a rigid, fixed-purpose building in 2025 will be obsolete by 2035—not because it’s old, but because it’s inflexible.
Three Pillars of Adaptable Hospital Design
Future-ready hospitals aren’t built on clairvoyance—they’re built on resilience through three core principles:
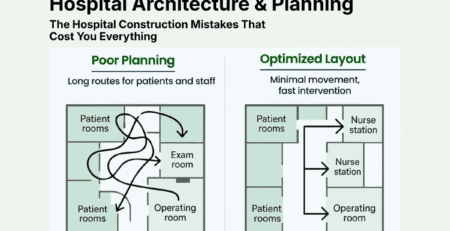
1. Flexibility: Convertible Spaces Without Structural Trauma
Design rooms to serve multiple functions throughout the building’s life without requiring demolition or major mechanical changes.
In practice:
- Patient rooms switch between general ward, step-down care, or isolation with minor modifications (movable headwalls, adaptable HVAC)
- Procedure rooms sized for today’s endoscopy or tomorrow’s robotic minor OT
- Diagnostic zones that expand or contract with demand
- OPD spaces converting to day-care beds by adding recliners
Key enabler: Design based on universal dimensions rather than specific functions. A 4m x 4.5m room with properly positioned utilities can be a consult room today, procedure space tomorrow, or observation bay next year.
The mindset shift: Stop asking “What will this room be?” Start asking “What could this room become?”
2. Standardization: Repeatable Modules, Not Custom Layouts
Use identical room modules repeated across floors and departments—standardized patient rooms, ICU bays, OPD consultation suites.
Why this matters:
- Clinical benefits: Staff work anywhere without relearning layouts. Standardized equipment positions reduce fumbling in emergencies. New staff orient 40-50% faster.
- Operational benefits: Stock one type of bathroom fixture, one headwall model, one ceiling grid. Fewer SKUs reduce inventory costs 30-40%. Housekeeping protocols become muscle memory, achieving 15-20% faster terminal cleaning.
- Economic benefits: Ordering 200 identical patient room packages gets better pricing than 200 custom rooms. Repetition means construction crews work faster with fewer errors.
- Common objection: “Standardization makes everything generic.”
- Reality: Standardization repeats the technical back-end (MEP, structural bay, room size), not the aesthetic front-end. The Taj Mahal and a factory both use standardized bricks.
3. Modularity: Build in Components, Not Permanence
Use pre-fabricated, factory-built components that can be installed, replaced, or reconfigured on-site with minimal disruption.
In practice:
- Pre-fabricated bathroom pods built in factories, craned into place
- Modular MEP racks that snap together on-site
- Demountable wall systems relocatable without demolition
- Integrated ceiling modules with lights, HVAC, and access panels
Why this matters during construction:
- 30-50% faster completion (factory work parallels site work)
- Higher quality control (factory-built components have lower defect rates)
- Weather-independent (reduces monsoon delays)
Why this matters during operations:
- Non-destructive changes (relocating walls takes hours, not weeks)
- Lower downtime (upgrading HVAC doesn’t require shutting entire floors)
- Convertible capacity (COVID taught this lesson—facilities that could adapt survived)
Real validation: India built 100-500 bed COVID facilities in 4-8 weeks using modular construction. Traditional construction would have taken 18-24 months. When the surge passed, many converted to step-down units or outpatient centers in 2-3 weeks—impossible with traditional brick-and-mortar.
The Financial Case: Why Flexibility Costs Less Than Rigidity
The predictable objection: “Modular and flexible design is expensive. We don’t have that budget.”
This reveals a fundamental misunderstanding. The question isn’t upfront cost—it’s total cost of ownership over 25-30 years, including construction speed, operational efficiency, and avoided renovation costs.
The Revenue Acceleration Factor
Scenario: 150-bed hospital with 4 OTs, projected ₹60 Cr annual revenue at full capacity.
Traditional construction (30 months): Start revenue Month 31. Years 1-3 total: ₹150 Cr
Modular construction (18 months): Start revenue Month 19. Years 1-3 total: ₹165 Cr
Advantage: ₹15 Cr additional revenue from 12 months earlier opening—typically exceeding the entire 5-15% capex premium for modular construction.
The Two Paths Forward
Path A – Traditional, Fixed Design:
- 3-8% lower upfront cost
- Optimized for today’s requirements
- Outcome in 15 years: Multiple disruptive renovations (₹2-5 Cr cumulative), inability to adopt new technologies, strategic constraints
- Result: Building limits what the hospital can become
Path B – Adaptable, Future-Proof Design:
- 3-8% upfront premium
- Designed for unknown future requirements
- Outcome in 15 years: 2-3 week reconfigurations (not 4-month renovations), technology-ready, strategic optionality
- Result: Hospital strategy drives building use, not vice versa
The Question for Leadership
“Are we willing to invest an additional ₹1-2 Cr today (3-5% of project cost) to ensure our hospital can adapt for 25 years without major disruption?”
Or:
“Are we comfortable spending ₹5-15 Cr over 25 years on multiple disruptive renovations while being constrained from strategic pivots our competitors can make?”
Conclusion: Building for Change, Not a Moment in Time
You cannot predict what healthcare will look like in 2045. No one can. But you can answer this:
“Is my building capable of adapting to whatever comes?”
In 2010, no one designed for telemedicine infrastructure. In 2015, pandemic surge capacity was unimaginable. In 2020, AI-powered diagnostics were experimental. Today, you’re making decisions about a building operating until 2045-2050.
You don’t future-proof a hospital by predicting what medicine will become. You future-proof it by ensuring the building can adapt faster than medicine evolves.
Design for change. Build in options, not constraints. Invest in resilience, not rigidity.
Do this, and your hospital will never be a stranded asset—it will be a platform for continuous evolution. Do this, and 15 years from now, when competitors are demolishing walls and shutting departments for major renovations, you’ll be reconfiguring spaces over weekends.
The choice is made now, in these 10 shell and core decisions. Choose wisely.



Leave a Reply