The 23-Hour Patient: Why Legacy Hospital Design is Your Biggest Revenue Leak
The most significant disruption in modern healthcare isn’t a breakthrough drug or a robotic surgeon; it is the radical shift in the site of care. Driven by advancements in minimally invasive surgery, anaesthesia, and payer pressure for cost-efficiency, a massive volume of clinical activity is migrating from traditional multi-day inpatient stays to short-stay or daycare models.
From interventional cardiology and orthopaedics to laparoscopic general surgery, the “daycare” is the new industry standard. However, while clinical protocols have evolved, hospital architecture remains stubbornly rooted in the past. Most facilities are still designed for long-stay, ward-centric care—a mismatch that results in nursing fatigue, bed-blocking, and significant financial underperformance.
For hospital promoters, COOs, and architects, the strategic question is no longer just about bed count; it is about velocity. Does your hospital design force patients into an inefficient Inpatient Department (IPD) model, or does it enable the high-throughput, short-stay care that defines modern profitability?
The Infrastructure Gap: Why Traditional Wards Fail Short-Stay Care
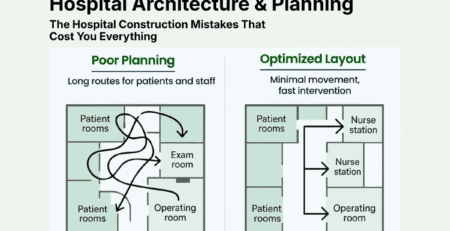
Conventional hospital layouts were designed for a different era—one characterized by long recovery timelines and mixed-acuity wards. When a 23-hour patient is placed in a traditional ward, the operational friction is immediate:
- Nursing Inefficiency: Nurses must traverse long corridors to manage a mix of high-acuity inpatients and low-acuity daycare patients. This “mixed-acuity” model dilutes focus and increases travel time.
- Capacity Misalignment: Using a high-spec inpatient bed for a cataract or endoscopy patient is an expensive misuse of real estate. It blocks that bed for potential high-margin emergency or complex surgical cases.
- The “Hospitalization” Tax: Traditional IPD workflows involve complex admission and discharge rituals. For a patient who only needs a few hours of recovery, these administrative hurdles create bottlenecks and lower patient satisfaction scores.
Design Showdown: Dedicated Short-Stay Unit (SSU) vs. Traditional Wards
To maximize Return on Investment (ROI), planners must shift from a “bed” mindset to a “bay” mindset. A dedicated Short-Stay Unit (SSU) acts as a high-velocity engine for elective procedures.
Comparative Efficiency Analysis
| Feature | Traditional Ward Model | Dedicated Short-Stay Unit (SSU) |
| Location | Dispersed floors, far from OTs | Immediate proximity to OT/Cath Lab |
| Patient Throughput | 1–1.5 patients per bed/day | 3–4 patients per bay/day |
| Staffing Model | Generalist nurses; mixed protocols | Specialized short-stay recovery teams |
| Turnaround Time | Slow (due to cleaning/admin lag) | Rapid (standardized prep & exit) |
| Revenue Potential | Diluted by high overheads | Optimized via high case volume |
The Power of Proximity
In a well-designed SSU, the travel distance between the Operating Theatre (OT) and the recovery bay should be under 50 meters. Minimizing transport time doesn’t just improve safety; it reduces the need for redundant staffing and allows for faster “Phase I” to “Phase II” recovery transitions.
The 23-Hour Patient Journey: An Architectural Blueprint
A profitable short-stay model requires a unidirectional, “frictionless” patient flow. Architecture must support the clinical workflow at every touchpoint.
1. Admission & Pre-Op Prep
Instead of the main lobby, short-stay patients should arrive at a dedicated SSU reception. Design should include Prep Pods—compact, private spaces for changing and IV initiation—located directly adjacent to the procedure rooms.
2. The Procedure-Recovery Link
The SSU should be self-contained. Once the procedure is complete, the patient moves to a Phase I Recovery Bay (high visibility for nursing) and then to a Phase II Step-Down Zone.
Design Tip: Use recliner-based recovery zones for Phase II. This signals to the patient and family that they are on the path to home, speeding up the mental and physical transition toward discharge.
3. Integrated Billing & Exit
The most common bottleneck in short-stay care is the discharge process. If a patient is medically ready but waits three hours for a bill, the throughput is ruined.
- Design Requirement: Integrated billing desks within the SSU zone.
- Operational Requirement: Tech-enabled documentation capture to ensure “Daycare” coding is accurate for insurance/TPA approval, preventing IPD-related claim rejections.
The Business Case: Why Velocity Equals Margin
From a financial perspective, the SSU model is superior because it decouples elective revenue from emergency volatility. When short-stay patients are mixed into general wards, an influx of emergency admissions can “bump” elective cases, leading to cancelled surgeries and lost revenue.
By segregating these flows, hospitals can:
- Increase OT Throughput: Faster bed turnover means surgeons can schedule more cases per day.
- Lower Labor Costs: Short-stay units allow for optimized nurse-to-patient ratios because the patient acuity is predictable.
- Enhance Asset Monetization: A recovery bay in an SSU costs less to build and maintain than a full IPD room but generates revenue at a much higher frequency.
Architectural Review Checklist for Hospital Promoters
If you are currently reviewing drawings for a new facility or a brownfield expansion, use this checklist to ensure your design is “daycare ready”:
- Is the SSU on the same floor as the OTs? (If not, are there dedicated elevators?)
- Are there distinct Phase I (monitored) and Phase II (step-down) zones?
- Can a patient walk from the procedure room to discharge without entering a general ward?
- Does the nursing station allow for 360-degree visibility of all recovery bays?
- Is there a dedicated billing and TPA desk within the unit?
Conclusion: Designing for the Future of Care
The future of healthcare medicine is “lighter, faster, and smarter.” As surgical techniques continue to advance, the percentage of patients requiring multi-day admissions will continue to shrink.
Hospitals that continue to build traditional, ward-heavy layouts are essentially building “stranded assets”—expensive infrastructure that will be underutilized as care shifts to the ambulatory sector. By integrating a dedicated Short-Stay Unit into your architectural plans, you aren’t just improving patient flow; you are building a high-margin, future-proof revenue engine.



Leave a Reply