The Hospital Construction Mistakes ThatCost You Everything
The Project That Should Have Been Straightforward
Let me tell you about a hospital project in Western India. Beautiful 150-bed facility. Well-funded promoter. Experienced architect. Everything looked perfect on paper.
Eighteen months after the planned opening, they were still scrambling for approvals. The fire department had rejected them twice. Staff had been hired and quit. The financial model had collapsed.
Total excess burn: ₹23 crore beyond the original budget. Eighteen months of lost revenue while paying EMIs, salaries, and storage fees.
This wasn’t bad luck. It was a predictable cascade of mistakes that I see repeated across hospital projects in India. Let me walk you through what actually goes wrong, not in a neat list of 27 numbered items, but in the messy, interconnected reality of how hospital projects actually fail.
The Foundational Mistakes (That Make Everything Else Harder)
The feasibility study you didn’t do properly
Everyone does “feasibility studies.” Most are garbage.
They hire a consultant who uses five-year-old demographic data, makes optimistic assumptions about occupancy rates, and presents a spreadsheet that shows great ROI. The promoter is happy. The bank is satisfied. Everyone moves forward.
What they missed: The new metro line that will shift catchment areas in two years. The competitor planning a 200-bed facility three kilometers away. The local insurance company’s shift toward smaller empaneled providers. The actual case mix in that area, which is 70% elderly with chronic diseases, not the surgical cases they’re planning for.
A hospital in Jaipur planned for 60% surgical cases based on outdated data. The actual demand in their area? 75% medical cases, 15% pediatric, 10% surgical. Their four expensive operation theaters sat underutilized while their medical ward was constantly overcrowded. They’re now spending money to convert two OTs into ICU beds.
Real feasibility means: Spend three months actually understanding your market. Talk to doctors, not just consultants. Visit competitor hospitals and count their cars in the parking lot at different times. Check insurance empanelment criteria. Model multiple scenarios, including pessimistic ones.
Budget plans that ignore reality
Every hospital project I’ve seen has a moment—usually around month 8-10—where everyone realizes the budget was fantasy.
The original budget covered:
- Land
- Building construction
- Basic equipment
What it forgot:
- Equipment is 50-60% of total cost, not 30%
- Installation costs another 10%
- Working capital for 6-12 months before revenue stabilizes
- All the specialized infrastructure (HVAC for OTs, medical gas systems, electrical redundancy)
- The inevitable cost escalations and delays
- The consultant fees nobody budgeted for
A hospital in Coimbatore budgeted ₹80 crore. Actual spend? ₹127 crore. The extra ₹47 crore came from:
- Equipment that cost 50% more than estimated (₹15 crore)
- MEP systems that weren’t properly specified (₹8 crore)
- AERB compliance retrofits (₹5 crore)
- Six-month delay carrying costs (₹7 crore)
- Working capital to stay afloat during ramp-up (₹12 crore)
Budget like a pessimist. Add 25-30% contingency. Assume everything will cost more and take longer than projected. You’ll be closer to reality.
The Site Selection Disasters
Choosing land based on price per square foot
I can’t count how many times I’ve seen this: Someone buys land because it’s cheap, then spends the next two years fighting the problems that made it cheap.
A hospital in Nagpur bought land at 40% below market rate. Seemed like a steal. Then they discovered:
- Water table was too high, requiring expensive deep foundations
- Approach road was narrow and couldn’t handle ambulances easily
- Power supply was inadequate, requiring ₹2 crore electrical infrastructure upgrade
- Flooding during monsoons required elevating the entire structure
- Neighbors filed objections to the hospital zoning change
The “savings” on land cost them ₹8 crore in fixes and a one-year delay.
Cheap land is cheap for a reason. Either it has infrastructure problems, accessibility issues, legal complications, or all three.
Ignoring what patients and ambulances actually need
Hospitals need different infrastructure than office buildings. But people treat site selection the same way.
What actually matters:
- Can an ambulance reach your emergency entrance in under two minutes from the main road?
- Is there space for patient drop-off that doesn’t block emergency access?
- Can two ambulances arrive simultaneously without chaos?
- Where do visitors park without blocking service areas?
- Is there a separate entrance for mortuary services?
These aren’t aesthetic concerns. They’re operational necessities. Get them wrong, and your ED becomes dysfunctional. A hospital in Indore has ambulances blocking their main entrance regularly because there’s no separate emergency access. The chaos is constant.
The Architectural Disasters That Haunt Operations Forever
Letting architects design without clinicians in the room
Here’s how hospital design usually happens: The promoter hires an architect. The architect designs a building that looks good. Then they try to fit hospital functions into it.
That’s backward.
A hospital isn’t architecture that happens to provide healthcare. It’s a clinical workflow machine that needs a building around it.
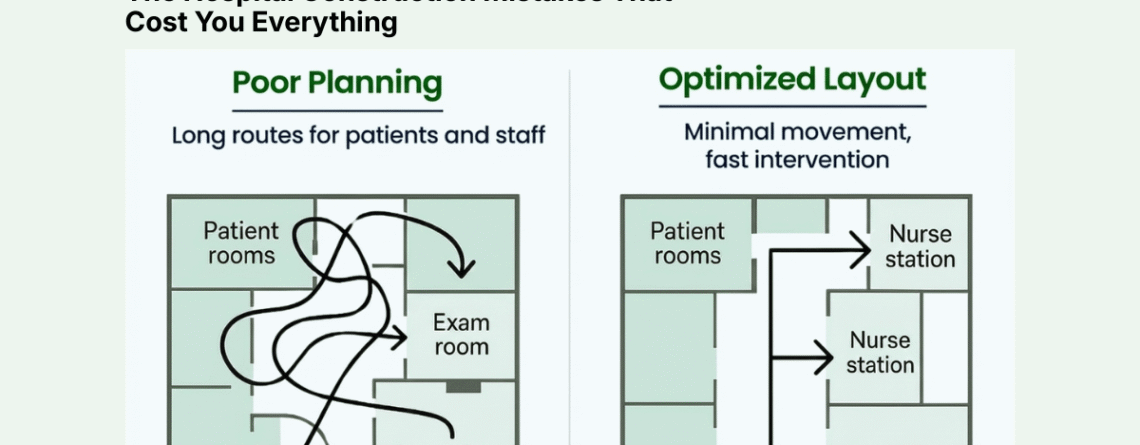
I’ve walked through dozens of hospitals where:
- The ICU is on a different floor from the OT, requiring critical patients to be transported via elevator
- Dirty utility and clean utility rooms are next to each other
- The OT sterile corridor crosses the dirty corridor
- Nurse stations can’t see patient beds
- Pharmacy is far from the nursing stations that need it
- Lab is far from patient care areas
- Staff cafeteria is somehow three floors away from the wards
Every one of these design flaws creates daily operational friction. Nurses walk extra kilometers. Delays happen. Contamination risks increase. Staff gets exhausted.
One hospital in Chennai realized their floor plan required nurses to walk 6 kilometers per shift just to complete routine tasks. That’s not just fatigue—it’s inefficiency that shows up as higher staffing costs and lower patient satisfaction.
Not planning for expansion you know will happen
Every single hospital I’ve worked with that’s successful has needed to expand within 3-5 years.
Every single one.
Yet most hospitals are designed with zero expansion capability. The building fills the entire plot. There’s no provision for adding floors. The MEP systems are sized exactly for current capacity with no overhead.
Then success creates a problem: You need to expand, but it’s impossible or prohibitively expensive.
Options become:
- Buy adjacent land (usually not available)
- Build on another site (splitting operations)
- Stay constrained and turn away patients
- Undertake massively expensive retrofits
A hospital in Lucknow wanted to add 50 beds. They can’t expand their building. Their DG set is already at capacity. Their medical gas system has no spare capacity. Their lifts are insufficient. Their sewage treatment plant is maxed out.
To add 50 beds, they need to upgrade everything—at roughly the same cost per bed as building new. They’re spending ₹5 crore for expansion that should have cost ₹2 crore if planned properly.
Design for your current need, but plan infrastructure for 50% growth. It’s cheaper to have excess capacity at the start than to retrofit later.
The MEP Nightmares That Cause Operational Failures
Under-specifying HVAC because it seems expensive
Hospital HVAC isn’t office building HVAC. It’s critical infrastructure.
OTs need 20-25 air changes per hour with HEPA filtration and precise temperature/humidity control. ICUs need negative or positive pressure depending on purpose. Isolation rooms need specific pressure differentials. Pharmacy storage needs climate control.
Cut corners here, and you pay forever.
A hospital in Ahmedabad installed standard commercial HVAC to save ₹40 lakh. Within six months:
- OT humidity was uncontrollable, leading to surgical delays
- ICU had infection control issues
- Pharmacy products were degrading in storage
Fixing it? ₹1.2 crore. Three months of disruption. Lost revenue and reputation damage.
HVAC isn’t where you cut budget. It’s life safety infrastructure.
Electrical systems designed by people who don’t understand hospitals
Hospitals need electrical redundancy that most buildings don’t require.
You need:
- Main power supply
- DG backup with automatic transfer
- UPS for truly critical loads (ICU, OT, server room)
- Separate circuits for critical vs. non-critical areas
- Proper grounding for medical equipment
Skip any piece, and you risk lives.
A hospital in Bhopal had their main power fail during surgery. Their DG didn’t start automatically (manual switchover). Their UPS covered only the server room, not the OT. The surgery had to be completed using flashlights from mobile phones while they scrambled to start the generator manually.
Miraculously, the patient survived. The hospital’s reputation didn’t.
The Equipment Planning Failures
Creating your equipment list after the building is designed
This happens constantly:
Month 1-12: Design and build the hospital
Month 13: Start thinking about equipment
Month 14: Realize the radiology room isn’t properly shielded
Month 15: Realize the CT scanner doesn’t fit through the door
Month 16: Realize the floor loading isn’t adequate for the MRI
Month 17: Start expensive retrofits
Equipment requirements must inform building design, not the other way around.
A hospital in Surat bought a beautiful MRI machine. When it arrived:
- The room wasn’t shielded to AERB standards (₹8 lakh retrofit)
- The floor reinforcement was inadequate (₹3 lakh)
- The dedicated electrical panel wasn’t installed (₹2 lakh)
- The cooling system was undersized (₹4 lakh)
The ₹4.5 crore MRI cost them another ₹17 lakh to install, plus three months of delay. Meanwhile, they’re paying interest on the equipment loan and storage fees.
Equipment planning needs to happen in parallel with building design, not after.
The Procurement Disasters
Lowest bid selection that costs you forever
The tender process in many hospitals:
- Create vague specifications
- Get bids
- Select the cheapest
- Spend years regretting it
A hospital in Vizag selected the lowest bidder for their entire ICU setup. The vendor saved money by:
- Using slightly inferior components
- Minimizing training
- Offering a weak service contract
- Importing from unreliable sources
One year in:
- Equipment breakdowns were 3x higher than comparable hospitals
- Service response time averaged 48 hours for critical equipment
- Consumables were expensive and sometimes unavailable
- Staff was inadequately trained and making errors
They calculated that the “cheap” vendor was costing them ₹15 lakh extra annually in downtime, repairs, and inefficiency. Over ten years, the cheap bid will cost ₹1.5 crore more than the expensive one.
Price is important. But lifecycle cost, service quality, and reliability matter more.
The Regulatory Catastrophes
Starting construction before getting all clearances
This is where optimism meets reality and gets crushed.
The thinking goes: “We’ll get the approvals as we go. How hard can it be?”
Very hard, it turns out.
A hospital in Kochi started construction with only the building permit. They figured they’d get other approvals later. Then:
Month 6: Fire department inspection reveals the design doesn’t meet spacing requirements. Requires partial demolition and redesign. Four-month delay, ₹35 lakh rework.
Month 12: Environmental clearance gets challenged by neighbors. Six-month legal battle. ₹12 lakh legal fees.
Month 15: Pollution control board objects to sewage treatment capacity. Requires upgrading the STP. Three-month delay, ₹18 lakh cost.
Month 18: Clinical establishment registration stalls because some infrastructure doesn’t meet state requirements. Need to retrofit multiple areas. ₹25 lakh cost.
The hospital that was supposed to open in 18 months opened in 31 months. The budget overrun was ₹90 lakh just from regulatory issues.
Get your approvals first. All of them. Even if it delays the start. The delays and costs of fixing problems later are always worse.
Assuming national standards apply everywhere
India has central regulations and state variations. People forget this constantly.
AERB is central. Fire codes are central. But clinical establishment registration is state-specific. Building codes have local variations. Pollution norms can be stricter at state level.
A hospital chain tried to use their Karnataka hospital design in Maharashtra. Seemed efficient—just replicate what works.
Except:
- Maharashtra has stricter biomedical waste segregation requirements
- Fire escape requirements differ slightly
- Clinical establishment registration has different documentation
- Local building codes require different structural specifications
They spent ₹50 lakh adapting the design and another three months getting approvals they didn’t expect to need.
Every state is different. Budget time and money for local compliance, even if you’re replicating a design.
The Commissioning Nightmares
Coordination failures that break everything
Here’s what hospital commissioning typically looks like:
Civil contractor finishes. MEP contractor starts. Biomedical contractor starts installing equipment. Everyone discovers problems simultaneously.
The medical gas pipes are where the cable trays need to be. The HVAC ducts clash with structural beams. The equipment won’t fit through finished doorways. The false ceiling height doesn’t accommodate medical pendants.
Everyone blames everyone else. Everything stops while they fight. Rework begins. Timeline extends. Costs escalate.
A hospital in Raipur had civil, MEP, and biomedical work happening simultaneously with no coordination. The result:
- 30% rework across all systems
- Three-month delay
- ₹2 crore in waste and fixes
- Relationships destroyed
Commissioning needs a sequencing plan with clear handoffs and inspections between phases. It needs one person coordinating everyone. Otherwise, it’s chaos.
The Operational Launch Failures
Opening without operational systems ready
A hospital in Vadodara was so eager to open that they cut corners on operational readiness:
- Staff hired one week before opening
- No orientation or training completed
- Supply chain contracts not finalized
- SOPs not written
- Biomedical maintenance team not in place
- No mock drills conducted
Week 1: Chaos. Staff didn’t know workflows. Supplies ran out. Equipment failures had no response protocol. Patients were endangered.
Week 2: They shut down non-critical services to sort things out.
Week 3: They started doing the preparation they should have done before opening.
Cost: Reputation damage that lasted years. Staff quit. Early patients had poor experiences and told everyone.
Opening a hospital isn’t ribbon-cutting. It’s the culmination of months of operational preparation—hiring, training, drilling, testing, refining.
What Actually Works
The hospitals that succeed do a few things consistently:
They build a multidisciplinary team from day one. Promoter, architect, clinician, biomedical engineer, MEP consultant, regulatory consultant—all in the room from the start.
They over-budget and under-promise on timelines. Add 30% to estimated costs. Add six months to projected timeline. You’ll be closer to reality.
They sequence everything carefully. Feasibility → Approvals → Design → Construction → Equipment → Commissioning → Staff → Testing → Launch. No shortcuts.
They make decisions for 10-year operations, not 1-year construction. Spending ₹50 lakh more during construction to save ₹5 lakh annually for ten years is smart.
They assume everything will go wrong and plan accordingly. Contingency budgets. Buffer time. Backup plans. Alternative vendors.
The Truth About Hospital Projects
Building a hospital is hard. Not “challenging” in an inspiring way. Hard in a “this will test everything you think you know” way.
There’s no perfect checklist. No foolproof sequence. Too many variables, too many interdependencies, too many things that can go wrong.
The projects that succeed aren’t the ones that avoid all mistakes. They’re the ones that:
- Expect mistakes
- Build in buffers
- Course-correct quickly
- Don’t compound errors with more errors
The Pune hospital I mentioned at the start? They eventually opened. Twenty-six months late. ₹35 crore over budget. They’re now profitable, but it took three years to recover from the rocky start.
They learned every lesson the expensive way. You don’t have to.
Before you break ground: Get every stakeholder in one room. Make a list of all the ways the project could fail. Then design your plan specifically to prevent those failures. The two hours you spend on this exercise will save you months of delays and crores in costs.

Leave a Reply