Frequently Asked Questions on Hospital Project Management & Consultancy
Q1. What’s your real timeline for completion?
We don’t promise generic months. Every project starts with a milestone chart built from actual site conditions —
Our 4-phase approach:
Phase 1: Excavation and Foundation
– Site survey completion
– Soil testing results
– Foundation sign-off criteria
Phase 2: Civil Construction
– Structural milestones
– Safety compliance checkpoints
– Weather contingency buffers
Phase 3: MEP Installation
– Electrical system testing
– Plumbing pressure tests
– HVAC commissioning
Phase 4: Fit-out and Commissioning
– Medical equipment installation
– Regulatory approvals
– Staff training completion
Each milestone includes:
– Clear dependencies
– Sign-off criteria
– Risk mitigation plans
We conduct weekly progress audits.
No surprises. No excuses. Just transparency.
Q2. How do you handle cost overruns?
Every single invoice gets checked against the original BOQ before payment. No exceptions.
Here’s our 3-step cost control framework:
Step 1: The 5% Rule
Any variance beyond 5% stops the payment process. The invoice goes to our cost estimator and site manager for joint review.
Step 2: Documentation First
Before any approval, we need written justification. Market price changes? Show us the data. Scope modifications? Show us the change order. No finger-pointing, just facts.
Step 3: Client Transparency
You see the same numbers we do. Real-time cost tracking, variance reports, and approval requests. No surprises at month-end.
The result? Our hospital projects average 3% under budget, not 25% over.
Most consultants hide cost overruns until it’s too late. We surface them early when you can still make decisions.
The difference between a successful hospital project and a financial disaster often comes down to one thing: catching problems while they’re still small.
Q3. Who manages vendor conflicts on site?
Most hospital projects fail because of one thing: vendor chaos.
Multiple contractors, consultants, and suppliers all talking past each other. Conflicting instructions. Finger-pointing when deadlines slip. Sound familiar?
Here’s what actually works: one person owns the mess.
Three vendors, two consultants, one very frustrated client. Everyone had “urgent” requests. Nobody knew who was really in charge.
The breakthrough came when we appointed a dedicated site coordinator.
→ Not a project manager juggling 10 other things.
→ Not a consultant who shows up twice a week.
→ A full-time person whose only job is managing vendor relationships on-site.
Here’s the framework that saved that project:
1/ One line of command: All vendor instructions flow through the site coordinator. No exceptions.
2/ One escalation path: Issues go to coordinator → project lead → client. Clean hierarchy.
3/ Everything documented: Site memos for every instruction. Email trails for every decision. No “he said, she said” disputes.
4/ Daily vendor huddles: 15-minute morning sync. What’s happening today? What’s blocking you? Who needs what from whom?
The results speak for themselves:
– Vendor disputes drops by 80%
– Project delays cut in half.
The magic isn’t in the process. It’s in having one person who wakes up every day thinking about vendor coordination. Someone who knows which contractor needs steel delivery by Tuesday. Who remembers that the electrical team can’t start until plumbing finishes zone 3.
Most firms try to save money by making this someone’s “additional responsibility.” That’s exactly backwards. The cost of vendor conflicts – delays, rework, relationship damage – is always higher than hiring the right coordinator.
Your hospital project deserves better than chaos.
Q4. Where’s your quality control process?
Most healthcare projects fail not because of bad planning.
They fail because quality control happens too late.
We’ve seen 100Crore hospital projects where quality checks started during construction.
By then, fixing problems costs 10x more than preventing them.
Smart healthcare leaders build quality control into every phase.
Not just at the end.
Here’s the framework that works:
- Phase 1: Design Quality Control
- Review architectural plans against clinical workflows
- Validate equipment specifications before ordering
- Check compliance with healthcare regulations early
- Phase 2: Procurement Quality Control
- Verify vendor certifications and track records
- Test critical equipment before delivery
- Audit supply chain for medical-grade standards
- Phase 3: Construction Quality Control
- Daily inspections with clinical input
- Real-time documentation of all changes
- Weekly quality meetings with all stakeholders
- Phase 4: Pre-Opening Quality Control
- Full system testing with actual workflows
- Staff training on new processes
- Patient safety simulations
The difference this makes:
Projects finish on time and budget
Equipment works from day one
Staff adoption happens faster
Patient safety risks drop significantly
Most organizations treat quality control as a checkbox.
The best ones treat it as their competitive advantage.
Your patients deserve systems that work perfectly from the start.
Not systems that get fixed after problems emerge.
Q5. How do you coordinate MEP systems with architecture and interiors?
We integrate MEP drawings during the schematic phase itself — not after walls go up.
Here’s how we coordinate MEP systems with architecture and interiors from day one:
Start integration during schematic phase
We don’t wait for the walls to go up.
MEP drawings get integrated when the building is still just lines on paper.
This prevents the nightmare of discovering your HVAC duct conflicts with a structural beam after construction starts.
Weekly coordination meetings are non-negotiable
Every week, structural engineers, MEP teams, and interior designers sit in the same room.
We review routing paths, clearance requirements, and access points. No exceptions.
Use clash detection tools before breaking ground
Digital models catch conflicts before they become expensive problems.
When the software shows your electrical conduit running through a water pipe, you fix it on screen – not on site.
On-site markups prevent rework
Field teams mark actual conditions against drawings.
Real measurements beat assumptions every time.
This feedback loop keeps everyone aligned with reality.
The difference this makes:
– 30% fewer change orders
– Faster project completion
– Lower overall costs
– Happier clinical teams who get functional spaces
Most teams coordinate MEP systems after design is “complete.”
The best teams coordinate from the very first sketch.
Q6. How do you ensure work stays within the client’s budget?
Our budget control runs parallel to design.
Here’s how we keep projects on track financially:
Real-time cost tracking with every design change
Most teams wait until design completion to check costs. That’s too late. We run cost assessments after each revision. Small changes add up fast in healthcare projects.
Transparent reporting at every milestone
Clients get detailed cost breakdowns weekly. No surprises. No hidden expenses. They see exactly where every dollar goes and why.
Early warning systems for budget risks
We flag potential overruns before they happen. Material price increases. Regulatory changes. Scope creep. Our clients know about budget threats weeks in advance.
Value engineering throughout the process
We constantly ask: “Can we achieve the same outcome for less?” Sometimes a different material saves 20%. Sometimes a layout change cuts construction time by months.
The result? Our hospital projects finish on budget 94% of the time.
Budget control isn’t about cutting corners. It’s about making smart decisions with complete information.
Your healthcare facility deserves both quality and financial discipline. They’re not mutually exclusive.
Q7. What documentation do you maintain during construction?
Here is what we maintain on every hospital project to ensure transparency and accountability:
- Digital material inspection logs
Every shipment gets logged with photos, specifications, and quality checks.
No material enters the site without proper documentation. - Daily progress reports
Visual updates with photos, milestone tracking, and issue identification.
These reports create a clear timeline of work completed.
- Bill comparison tracking
We document every invoice against original quotes and budgets.
This prevents surprise costs and keeps spending transparent.
- Vendor quote management
All supplier communications, pricing changes, and delivery schedules are stored digitally.
This creates accountability across the supply chain.
- Real-time inventory tracking
Materials on-site are tracked from delivery to installation.
This prevents waste and ensures quality control.
The game changer is our shared dashboard system.
Clients get real-time access to all documentation.
Hospital owners can see progress updates, budget status, and quality reports anytime.
No waiting for weekly meetings or email updates.
This transparency builds trust and prevents the finger-pointing that destroys healthcare construction projects.
When documentation is done right, audits become simple. Compliance becomes automatic. And projects finish on time and on budget.
Q8. How do you verify contractor bills and claims?
Most people get contractor billing wrong, and it costs them big time.
They approve bills based on trust alone.
But in complex healthcare projects, trust alone is not enough.
You need verification, validation, and clear audit trails.
That is why we use a three-step verification framework that has saved my clients millions in disputed claims:
Step 1: Quantity Verification
Check delivered quantities against work orders.
Cross-reference with site delivery receipts.
Flag any discrepancies before processing.
Step 2: Site Validation
Physical inspection of completed work.
Photo documentation of progress milestones.
Quality checks against technical specifications.
Step 3: PO Cross-Reference
Match all claims against original purchase orders.
Verify rates and terms are consistent.
Ensure no scope creep without proper approvals.
Here’s a real example from a 200-bed hospital project:
A contractor submitted bills for 500 cubic meters of concrete.
Step 1 – caught that delivery receipts showed only 450 cubic meters.
Step 2 – revealed the remaining 50 cubic meters were substandard and rejected.
Step 3 – confirmed the PO allowed for quality-based deductions.
Result: We avoided paying for 100 cubic meters of unusable concrete.
Why this matters:
Most billing disputes happen because verification was skipped upfront.
Clean verification means clean expenditure tracking.
Proper documentation protects you during audits and disputes.
The framework works because it creates accountability at every step.
Contractors know their work will be verified.
Finance teams get clean, traceable approvals.
Project managers avoid surprise cost overruns.
Only verified quantities move forward for approval.
Everything else gets queued for resolution.
No exceptions, no shortcuts.
Q9. What’s your escalation process when issues arise?
Every problem has an owner.
Here is the system we use for healthcare infrastructure projects:
Every problem gets an owner within 24 hours.
No exceptions. No passing the buck.
Issues are categorized immediately:
- Urgent: Safety, compliance, or critical path items
- Routine: Everything else that can wait
Each category has strict response times:
- Urgent issues get same-day attention
- Routine items are addressed within 72 hours
We track everything until closure.
Not just logged. Not just assigned. Resolved.
Unresolved items automatically appear in the next weekly review.
No hiding. No forgetting. No surprises.
Why this matters in healthcare projects:
A delayed medical gas installation can push back an entire ICU opening.
A compliance issue caught late can trigger regulatory reviews.
Equipment delivery problems can cascade through multiple departments.
The cost of poor escalation is not just money. It is a patient care capacity.
Most teams think escalation means shouting louder or calling more meetings.
Real escalation means clear ownership, defined timelines, and systematic follow-through.
When everyone knows who owns what and when it needs to be done, problems get solved instead of managed
Q10. Do you help with procurement and vendor selection?
Yes, we help with procurement and vendor selection—especially in high-stakes healthcare infrastructure, where rushed decisions can cost crores.
Most healthcare leaders get procurement wrong by skipping the groundwork. Speed without strategy is expensive. You need clarity, comparison, and compliance visibility.
That’s why we use a three-part procurement framework to untangle complex vendor decisions:
Compare: Detailed vendor comparison sheets across all critical metrics
Negotiate: Favorable rates backed by market intelligence and performance data
Recommend: Shortlisted vendors based on proven performance and compliance standards
Real-world example from a recent hospital expansion project:
- Compare: Evaluated 12 medical equipment manufacturers across 15 criteria (compliance history, service response times, total cost of ownership).
- Negotiate: Uncovered 18% price variations for identical equipment; secured rates 12% below initial quotes through structured negotiations.
- Recommend: Delivered a final shortlist of 3 manufacturers, each fully compliant and performance-vetted.
Why this matters:
Procurement failures rarely stem from the vendor—it’s incomplete evaluation and rushed decisions. Our framework brings clarity before contracts are signed. You make the final call, but our groundwork eliminates costly trial and error.
Result: Significant time savings + drastically reduced procurement risk.
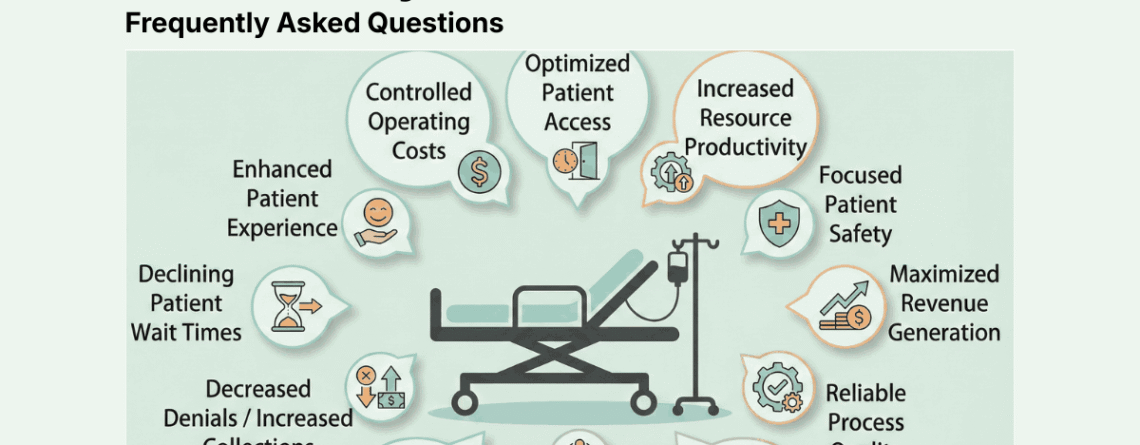
Q.11 What makes us different from other Hospital Consultants?
Most hospital consultants sell you the same recycled playbook.
We don’t.
While others push quick fixes and generic solutions, we dig deeper into what actually moves the needle for healthcare organizations.
Here’s what makes our approach different:
- We start with data, not assumptions. Before recommending anything, we spend 15–30 days analyzing your current systems, patient flow, and operational bottlenecks. Most consultants skip this and jump straight to their standard playbook.
- We focus on sustainable change, not temporary wins. Other firms implement solutions that look good on paper but collapse after 6 months. We build systems your team can maintain and improve long-term.
- We work with your people, not around them. The biggest consulting mistake? Ignoring the staff who do the actual work. We train your existing team to own the changes—so you’re never dependent on outside help.
- We measure what matters. Patient satisfaction scores are nice. We track the metrics that hit your bottom line: readmission rates, average length of stay, staff turnover, and operational efficiency.
- We stay until it sticks. Most consultants deliver a report and vanish. We provide 60 days of implementation support to ensure changes take root in your organization.
The result?
Our clients see measurable improvements that last years, not months.





Leave a Reply